Introduction:
Previous studies have demonstrated that allogeneic haploidentical (haplo) peripheral blood stem cell transplantation (PBSCT) with post-transplant cyclophosphamide (PTCy) yields improved progression free survival (PFS) when compared to haplo bone marrow transplant (BMT) with PTCy, attributable to lower relapse without an increase in non-relapse mortality (NRM) (Bashey, et al. JCO. 2017). However, haplo PBSCT results in higher rates of graft-versus-host disease (GVHD) which may negate these benefits in older patients who are more susceptible to transplant related toxicity. Thus, evaluation of the outcomes of haplo PBSCT with PTCy in older patients is warranted.
Methods:
We retrospectively evaluated 121 adult patients with hematologic malignancies treated at the Moffitt Cancer Center with allogeneic T-cell replete PBSCT from a haplo donor followed by PTCy-based GVHD prophylaxis. Data were extracted from the Moffitt BMT Research & Analysis Information Network (BRAIN) database. Myeloablative (n=70, 58%) and reduced intensity (n=51, 42%) conditioning regimens were included. Transplant related outcomes were compared between two age groups: <60 years (n=66) versus >60 years (n=55). Associations with transplant related survival outcomes were assessed using univariate and multivariate Cox proportional hazard survival models. Fine and Gray regression models were used to assess associations of transplant related endpoints with competing risks. Kaplan-Meier curves and cumulative incidence function curves were also plotted.
Results:
The median age at the time of transplant was 42 years (range: 20-59) for the younger group and 66 years (range: 61-75) for the older group. The median follow-up was 17 months (range: 2-53) for the entire cohort. Younger patients were more likely to receive myeloablative conditioning (83% versus 27%, p<0.001). Baseline characteristics were otherwise similar.
Neutrophil engraftment (>500/uL) by day 30 did not differ significantly between the younger and older group (98% versus 93%, p=0.26). However, the median time to neutrophil engraftment was faster in the younger group versus the older group (16 versus 21 days, p<0.001). Platelet engraftment (>20,000/uL) by day 90 was achieved in 92% in the younger group versus 76% in the older group (p=0.03). The time to platelet engraftment was faster in the younger group: 28 days versus 36 days (p=0.006). At day 100, the cumulative incidence (CuI) of grade II-IV acute GVHD in younger patients was 42% (95% CI 29-61%) and for older patients was 35% (95% CI 22-55%, p=0.82). The CuI for grade III-IV acute GVHD for the younger and the older groups were 8% (95% CI 4-25%) and 15% (95% CI 7-38%, p=0.23), respectively. At 2 years, the CuI of chronic GVHD was 67% (95% CI 55-82%) for younger patients versus 56% (95% CI 38-82%) for older patients (p=0.20). NRM for the younger group and the older group, respectively, was 6% (95% CI 2-16%) versus 19% (95% CI 11-34%) at 100 days and 14% (95% CI 6-30%) versus 22% (95% CI 13-37%) at 2 years (p=0.17). The CuI of relapse at 2 years was not significantly different between the two age groups, with the younger recipients having a CuI of 42% (95% CI 20-60%) and the older group 31% (95% CI 17-56%, p=0.70). The 2-year DFS was similar between the younger and older group, respectively: 51% (95% CI 36-66%) and 53% (95% CI 37-70%, p=0.72). Similarly 2-year overall survival (OS) for the younger group was 59% (95% CI 44-74%), while the older group was 66% (95% CI 52-80%, p=0.92).
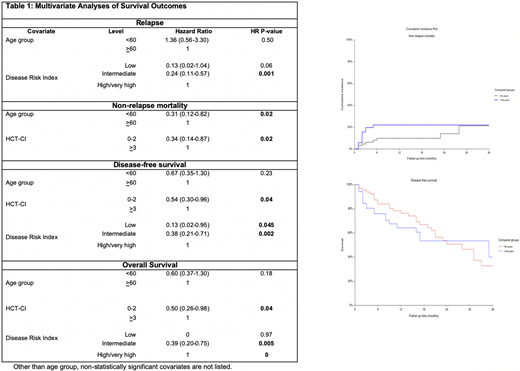
In multivariate analysis, NRM was superior in the younger group (HR=0.31, 95% 0.12-0.82, p=0.02). Otherwise, age was not associated with engraftment, risk of acute or chronic GVHD, relapse, DFS, or OS.
Conclusion:
Our results demonstrate that outcomes following allogeneic haplo PBSCT with PTCy in patients >60 years approximate outcomes in patients <60 years. While NRM was inferior in the older patient group, this difference did not result in significant differences in long term OS or DFS. Instead, other variables such as the hematopoietic comorbidity index and the disease risk index were better indicators of survival outcomes. Additionally, these survival outcomes with haplo PBSCT with PTCy appear to be similar to prior published data with haplo BMT with PTCy in older patients (Kasamon, et al. JCO. 2015). Based on this study, haplo PBSCT with PTCy is an appropriate transplant platform for elderly patients.
Khimani:Bristol Myers Squibb-Moffitt-Alliance: Research Funding. Nishihori:Novartis: Other: Research support to institution; Karyopharm: Other: Research support to institution. Pidala:Syndax: Consultancy, Membership on an entity's Board of Directors or advisory committees; CTI Biopharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; Takeda: Research Funding; Janssen: Research Funding; Johnson and Johnson: Research Funding; Pharmacyclics: Research Funding; Abbvie: Research Funding; BMS: Research Funding. Bejanyan:Kiadis Pharma: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal